The accelerated development of COVID-19 vaccines is a triumph of science, and governments will soon turn their attention on ways to achieve the highest possible rates of vaccination. That requires a multi-factorial and multi-stakeholder approach, involving high vaccine confidence, robust logistics, sustainable financing, high access to healthcare facilities, equitable distribution and training health professionals, among others.
Increasing public trust and confidence in the COVID-19 vaccine requires another multi-factorial and multi-stakeholder approach, which must start well before the vaccine arrives in the health clinic. Unfortunately, these efforts are complicated by vaccine hesitancy. Vaccine hesitancy is defined as a delay in acceptance or refusal of vaccination despite availability of vaccination services, and is deemed as one of the top ten health threats in the world today by the World Health Organization (WHO).
Despite the severity and personal impact of the COVID-19 pandemic, the availability of a vaccine does not necessarily equate to its de facto acceptance and utilisation. As a measure to achieve the highest possible rates of vaccination, should governments then deploy mandatory vaccination as a public health tool?
This policy brief seeks to answer this question by focusing narrowly on mandatory vaccinations for COVID-19. It considers the vaccine hesitancy landscape during COVID-19, examines the effectiveness of mandatory vaccinations, provides arguments for and against mandatory vaccinations, and considers the ethical dilemmas for countries as they consider this option.
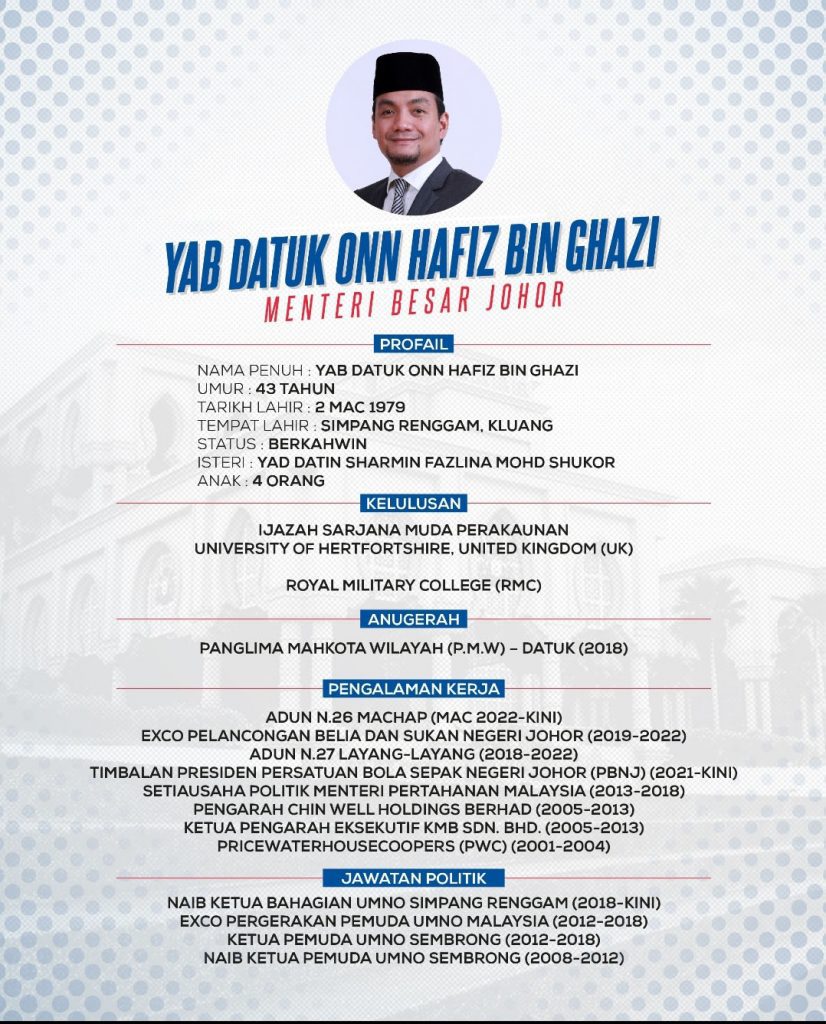
By
Dr Khor Swee Kheng
Visiting Fellow
Institute of Strategic and International Studies (ISIS) Malaysia
Nurul Ezzaty Hasbullah
Rhodes Scholar
MSc in International Health and Tropical Medicine, University of Oxford